Neuroma and phantom limb pain

Our private Neuroma and phantom limb pain services are provided at the Royal Free Hospital, Hampstead.
To find out more about our hospitals click here:
Pain management after an amputation is challenging. Amputation of a limb may result in pain which is amongst the most severe a person may ever experience. The pain experienced after amputation is the result of direct damage to the bones and soft tissue as well as nerve related (neural). The neural pain is the result of injury to the peripheral nerves and loss of feedback to the central nervous system from the absent limb. These varied sources of pain leads to a very mixed form of pain which can require a very varied approach for treatment, including both surgical and non-surgical modalities.
Moreover, the burden of pain after amputation persists not only in the short term, but also in the years and decades after surgery. Fortunately, every patient is unique and not every patient who has an amputation suffers from significant pain requiring specific intervention.
In terms of nerve related pain, amputees may experience two types of stump pain. The first is Neuroma Pain (NP) and the second is Phantom Limb Pain (PLP).
Neuroma Pain
can affect up to 80% of patients after an amputation and daily pain is reported in nearly half of all amputees. However, for most amputees, neuroma pain does not prevent them from using a standard, socket-fitted prosthesis and the pain is something they simply learn to tolerate.
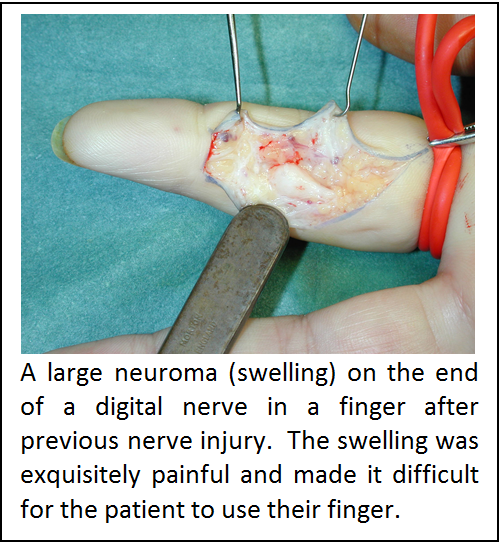
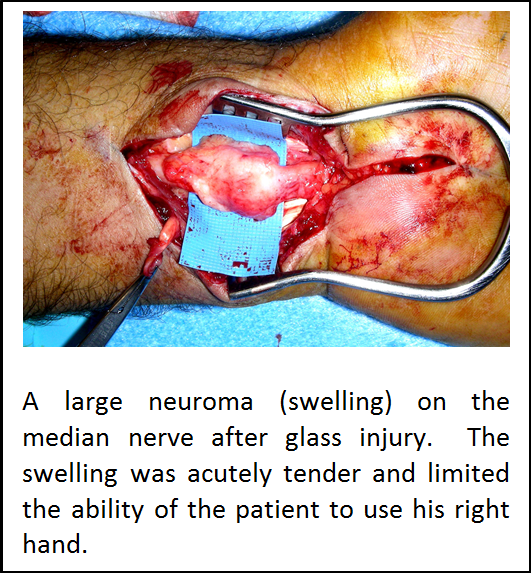
A neuroma is a painful lump of scar tissue that forms at the end of an amputated nerve. It represents a disorganised growth of nerve endings at the end of the nerve and can often occur after a nerve is partially or completely disrupted by an injury — either due to a cut, a crush, or excessive stretching (this is the mechanism of a typical brachial plexus injury). Typically, a neuroma is a ball-shaped mass (which varies in size from a golf-ball to a pinhead, depending on the size of the nerve from which it arises) which forms at the site of the injury. Pain is caused by tapping the neuroma or by direct pressure, resulting in pain at that site accompanied by an uncomfortable sensation of electric shocks which may travel up the residual limb. Painful neuromas are particularly common after amputations in the hand and upper extremity (arm) and in the lower extremity (leg) but less so in the thigh.
The therapeutic options for treatment of a neuroma are becoming increasingly clear. The neuroma forms because of a thwarted attempt by the peripheral nerves to reconnect with the sensory and motor end organs in the amputated part. As a result, they become very sensitive. Traditional treatments have relied on burying the nerve ends to try and cushion or discourage formation of a neuroma. Review of these traditional methods has shown that these options are not effective. At Relimb™ we adopt a different approach and aim to provide the peripheral nerves with a target end-organ to which the healing nerves can become connected.
This reduces the sensitivity of the peripheral nerves and prevents the neuroma from re-forming. Currently, there are only two ways in which to achieve this objective. The first is Targeted Muscle Reinnvervation (TMR) surgery and the second is to use a Regenerative Peripheral Nerve Interface (RPNI). Details of these surgical procedures are given elsewhere in this website.
Phantom Limb Pain (PLP) is also common. All amputees experience phantom limb sensation (the perception that the amputated part is still present). However, a smaller percentage (figures vary from 10 – 30%) experience an abnormal perception of their amputated limb which amounts to pain. Risk factors predisposing to the development of PLP include; significant pain in the amputated part prior to the amputation, standard prosthesis use, lower limb amputations and bilateral amputations.
Amputees often describe PLP as a “burning”, “stabbing”, “twisting”, “cramping”, “crushing” or “throbbing” pain arising in some part of their amputated limb. Therapeutically, this type of pain is hard to control but there is increasing evidence that the root cause is the loss of normal feedback from the amputated part to the central nervous system.
The therapeutic options for control of PLP are also becoming increasingly clear. To restore feedback to the central nervous system, patients can use a variety of surgical and non-surgical approaches. This includes TMR or RPNI surgery or non-surgical methods such as mirror therapy or augmented reality. Relimb is happy to discuss all of these options with you in your consultation.
