Osseointegration aftercare

Our private Osseointegration aftercare services are provided at the Royal Free Hospital, Hampstead.
To find out more about our hospitals click here:
After osseointegration surgery in the upper or lower limb, you will receive a combination of pain medications depending on your specific needs. This may include the use of a patient controlled analgesic device (PCA) or a continuous infusion of local anaesthetic through an in-dwelling catheter. Alternatively, you may be able to manage your pain needs with oral medication alone (e.g. tramadol or oxycontin).
The aim is to try and convert you to oral analgesia as quickly as possible so that you can have a clear enough mind to allow you to commence your rehabilitation as soon as possible.
You will stay in hospital for a maximum of 3 – 5 days. However, exceptionally, some patients may feel able to go home on the same day as the surgery. All patients are unique in terms of their perception of pain and you will simply have to see how you feel on the day after your surgery.
Wound care
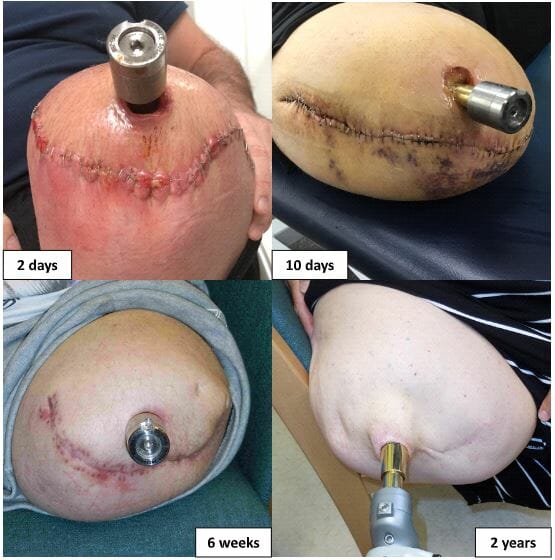
Immediately after surgery, we apply absorbent gauze which is secured over the stapled wound with an adhesive dressing (e.g. Mefix™). This will be left in place for a maximum of 1 week after surgery. Do not worry if the dressing becomes soaked with blood. Despite appearances, all will be well under the dressing and it can be easily replaced without affecting the long-term outcome of your treatment. Importantly, if you wish, you can shower immediately after surgery without affecting the final outcome. Running water is fine but soaking your wounds in bathwater is a bad idea. If you do shower, then any dressings will come off and they will need to be replaced.
If it proves necessary to replace your dressing before discharge, we will normally apply a simple adhesive dressing such as Mepore™. Again, this can be easily replaced either by the nursing staff or yourself. If there has been minimal discharge, you can leave the original dressing in place for up to one week. The main aim is to allow any discharge from the stump to leak out rather than accumulate inside the wound.
After one week, we recommend allowing your wound to be exposed to the air and light on a regular basis, for an hour or two every day. You will only need to apply a dressing when you are out and about outside the home. Skin staples will be removed partially at 3 weeks and completely at 4 weeks.
More detailed advice on longer-term aftercare is given elsewhere on these webpages.
Limb Pain
Pain after osseointegration surgery can be the result of many factors and treatment needs to be targeted at the root cause of this issue. These causes could include:
- Muscular pain. This can occur due to direct surgical trauma to the muscles and because many of the muscles in the stump are being used for the first time since the initial amputation. Muscular pain varies in severity and duration based on your level of activity, the degree of disuse and muscle wasting, and the time required to build these muscles back.
- Enthesopathy. This is an inflammatory process that occurs at the site of insertion of the muscles into the periosteum of your residual bone. Normally, your muscles are attached to the bone by tendons. After an amputation or after insertion of a bone-anchor, the muscle ends are sutured to the periosteum. When you start to mobilise, the muscles will pull on the periosteum causing pain – because the periosteum is exquisitely sensitive. The amount of pain you experience is often related to how vigorous you are with your exercise and it is usually distinct from any bony pain. To treat the inflammation, it is sometimes necessary to go more slowly with your rehabilitation or to have a series of steroid injections into the area. If it occurs, enthesopathy related pain usually begins at 3 – 6 months after insertion of the bone-anchor.
- Bone pain. Immediately after surgery, you should not experience any pain in your residual bone if the bone-anchor has been fixed securely in the bone. However, you should know that the osseointegration process takes a minimum of 6 weeks and up to 3 months to be complete. If you do experience pain when your bone-anchor is compressed, pulled or twisted after surgery, then there are a number of possibilities.
- The bone-anchor has not yet osseointegrated – discuss this with your surgeon. Often, it is just a question of waiting for a few more weeks until this type of pain disappears. Once it has settled, you will be able to begin the loading process in earnest.
- There is a fracture in the bone. Small fractures may sometimes occur during the process of insertion of the bone-anchor – discuss this with your surgeon. These fractures will heal within a few weeks and then the pain will disappear. It will not compromise the long-term outcome of your treatment.
- There is a deep infection of the implant. This last scenario will only occur in the months or years after surgery. We advise you to discuss this possibility with your surgeon. The risk of a deep infection of an OPL implant is <1.5% at 10 years.
- Pain due to bony spurs or heterotopic ossification is generally eliminated by removal of this extra bone – because these areas are no longer compressed in a socket.
- Skin irritation is generally eliminated but may be replaced by pain arising from the stoma (i.e. the opening where the implant protrudes through the skin). This may need temporary treatment with local anaesthetic creams or patches (e.g. lidocaine).
- Neuroma pain usually disappears after surgery but may recur later (3 – 6 months after surgery) if the only treatment performed during the osseointegration surgery was standard traction neurectomy. If TMR surgery was performed simultaneously to address a pre-existing neuroma, then your neuroma pain will disappear immediately after surgery. However, you may temporarily experience a significant increase in phantom limb pain lasting for 3 – 6 months after surgery.
- Phantom limb pain (PLP) is difficult to treat but is thought to be the result of a loss of feedback from the amputated part to the central nervous system (CNS). Many amputees (up to 30%) who undergo osteointegration surgery also report significant improvements in PLP within 3 – 6 months after treatment and this is probably the result of osseoperception providing feedback from the absent limb to the CNS. TMR surgery achieves a similar but more consistent effect for more amputees.
Osseointegration
Get in touch
